Pain is one of those experiences that we all have, but don’t really understand well. Having worked in the area of pain for over 30 years, some of us are still learning and trying to get our heads around how it all works. It is not as simple as it is portrayed – a sensation received from the body that is proportional to the state of the tissues. It is much more complicated than that, especially when it comes to persistent pain. So we can appreciate that when it comes to explaining some of the up-to-date, modern theories of pain experience, some patients struggle to accept them. This series of articles will outline (hopefully in simple terms) the process involved in Pain Reprocessing Therapy, and the first step is to understand what pain is and what it means.
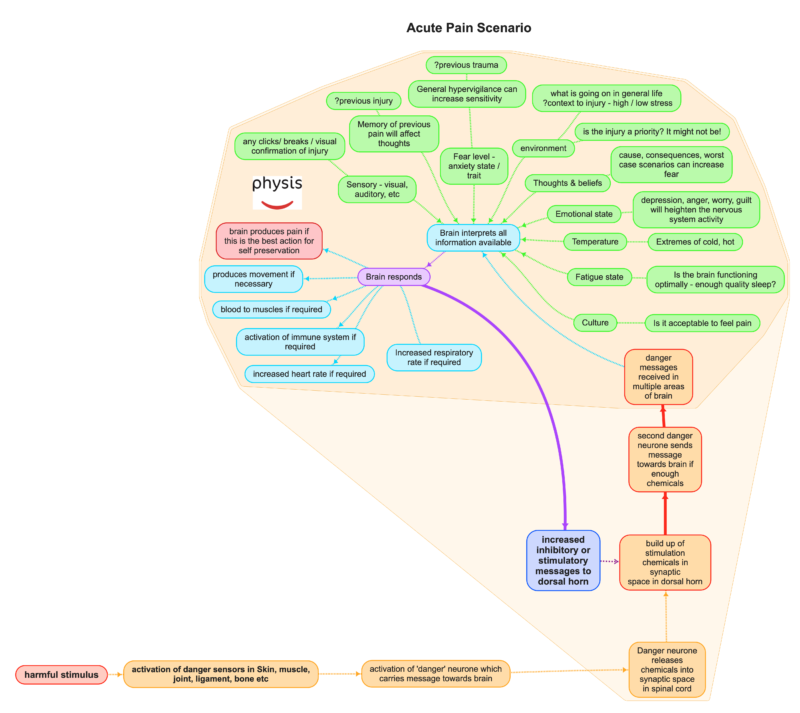 Pain is a danger alarm that goes off in your brain. Let’s consider what happens when you touch a hot stove in an acute pain scenario. Signals from your skin travel to your brain through nerves relaying danger information regarding the state of the tissues. This information from the skin is processed in the brain, and the end result might be that the alarm (pain) is set off, bringing your attention to the area. As a result, you protect yourself from damage by withdrawing your hand. This mechanism is easy to accept and is what we generally think of when we think of how pain works – pain generated from stimulation of the nerve endings in our skin or muscles. This type of pain is referred to as ‘nociceptive pain’ and occurs when the alarm system is working well.
Pain is a danger alarm that goes off in your brain. Let’s consider what happens when you touch a hot stove in an acute pain scenario. Signals from your skin travel to your brain through nerves relaying danger information regarding the state of the tissues. This information from the skin is processed in the brain, and the end result might be that the alarm (pain) is set off, bringing your attention to the area. As a result, you protect yourself from damage by withdrawing your hand. This mechanism is easy to accept and is what we generally think of when we think of how pain works – pain generated from stimulation of the nerve endings in our skin or muscles. This type of pain is referred to as ‘nociceptive pain’ and occurs when the alarm system is working well.
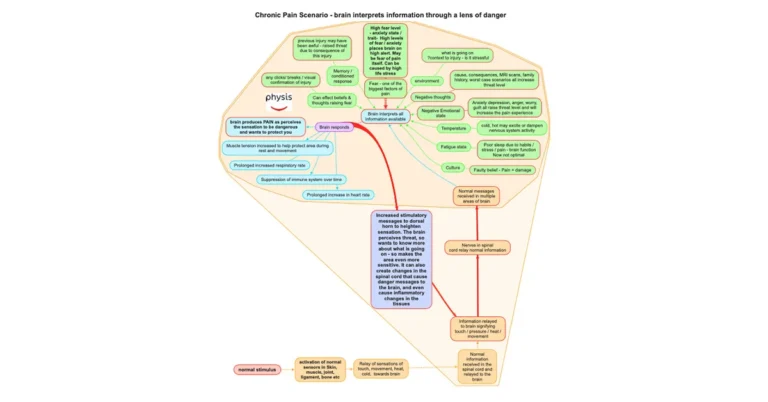
But pain is the ‘alarm’ part of the scenario. It doesn’t have to be triggered and sometimes it rings even when there is no stimulation from the skin or other tissues. The activity in the nerves relaying the information to the brain is not actually pain, this is called nociception, and it is not the same as pain. You dont feel the messages coming up the nerves. Nociception is represented as the orange boxes in the diagram above. Pain only occurs in the brain (and is the red box), and can occur with or without nociception. As you can see above, it is actually an output of the brain and occurs in response to lots of processing. This is the bit that we often get stuck on. The intensity of the pain, (or the volume of the alarm) will fluctuate depending on lots of factors the brain considers. These include your emotional state, your thoughts around what is happening, how tired you are, any previous memory of previous pain problems, your frustration levels, the consequence of the situation you find yourself, etc. All this information is instantly processed and a decision is made in your brain as to the best course of action. If your brain decides it needs to protect you, it will create enough pain to make you pay attention to the situation / injury.
However, sometimes the danger alarm (pain) is activated in the absence of structural tissue damage (and nociception), and sometimes the brain interprets safe / normal messages from the body (such as touch or stretch) as being dangerous and as a result produces pain. The pain is real. It is always real. It is produced and amplified by your brain. Even in the absence of danger messages (nociception) from the tissues, the pain is as real as if you have just cut yourself. The fire alarm (pain) is going off, but there is no fire. The fire alarm would be real and just as annoying. In fact more annoying, because it is not as easy to turn off.
There are many recorded cases in history demonstrating the existence of no pain in situations of severe tissue trauma, and cases of severe pain where no tissue injury exists. The alarm in your brain is there to protect you, but is not always a good indicator of what is going on in the tissues and sometimes the brain overprotects you producing pain when it doesnt need to.
So, pain is actually a very poor indicator of the state of the tissues. The intensity of the pain you feel is not proportional to the state of the tissues in your body. It’s the other factors that influence the degree of pain you experience. We continuously see patients that bend over or wake with severe pain, being completely debilitated by the pain, but after a session of treatment, the pain has completely eased to a minimal level. Although we would like to think our selves as miracle workers, we are not healing the tissues within minutes, but affecting the pain processing from tissues to brain.
Conversely, we see people where the pain exists long past the length of time you would expect the body tissues to have healed, and when we look at the state of the joints and the muscles, there is nothing out of the ordinary to see. The tissues have healed, but the pain persists. Most injuries will improve or resolve within 3 months, so when the pain persists past this period, we need to consider the potential for the pain to be due to a processing problem, rather than purely due to the damaged tissues not healing. This type of pain has a few labels including primary pain, nociplastic or neuroplastic pain and it is the most common type of pain in persistent pain problems. It is considered a malfunction in an intact pain system. In this type of injury, treatments to the tissues are not very effective as often the muscles, ligaments, tendons have healed or are quite normal.
The third type of pain is neuropathic pain and this occurs when there is disease or damage to the pain system. This might be due nerve injury, diabetic neuropathy, shingles, or stroke. As part of your examination, we are trying to consider your story, your physical presentation and as part of your diagnosis, trying to work out if your pain is nociceptive, neuropathic, or neuroplastic or a combination. Recognising which types of pain are dominant in your presentation, helps us decide what treatments will be best for you and how to best manage you.
As far as pain types go, most clinicians are very good at treating nociceptive pain – we treat the tissues and the problem will get better. Neuropathic pain is easy to diagnose and requires a multidiciplinary approach to manage it. Neuroplastic pain is not well recognised, even in the medical profession and needs a specific type of approach. Opiod medication (Codine / Tramadol / Oxycodone / Fentynl etc) is ineffective in treating this type of pain, and actually can make the problem worse.
Here are a couple of other resources that might help: